LIVING WITH THE ANXIETY OF HAVING A CHILD WITH NF
JESSICA JEMENTE

A few hours ago I was fine... Well, okay, not fine but I was suppressing/managing my anxiety to the best of my ability, like I do on a normal basis. BUT last night it all hit me. This is what life is like now. It is fear, sadness, the feeling of being lost, angry, confused and helpless.

This is having a child with an incurable medical condition. Not a medical condition that entails just ONE type of illness or symptom but a terrifying genetic disorder that causes countless symptoms, illnesses, pain and disabilities and there’s no way to know when/if they will show up or how severe.
So, when my beautiful daughter complains on and off over a few weeks that her “tummy hurts” pointing to her chest or that her legs hurt or I see new bumps or spots on her skin, my heart sinks. I begin to think of worst-case scenarios and my stomach is in knots. I quickly think about which specialist I need to contact and if this is something that we should see her regular pediatrician for (because she is, after all, a growing toddler) or could it be something more growing inside her, something out of place, a tumor, the list goes on...
My husband and I talk it over and over and over. I reach out to my fellow NF parents and search MANY posts related to what I see my daughter experiencing. Then book an appointment and talk to the doctor about everything that’s been leading up to this. I rack my brain trying to remember every diagnosis, struggle, pain, treatment, medication and supplement she’s taken at EVERY appointment. It’s exhausting and I have to relive the pain this disorder is causing every time but I don’t want to miss anything that could be relevant. If I do forget to mention something I am so disappointed in myself for not memorizing every detail of her health by now or not preparing my questions better beforehand. We discuss our plan going forward and what we will do now (X-ray? MRI? Will she need anesthesia again? EEG? Blood work? See another department? Try a med?). Will it be diagnostics today or just monitor this time?
We go home and try to resume our normal day to day life. Then it happens again...Something else pops up. Mya seems to be in pain, she’s walking a little strange, she rolls her eyes, and twitches in a funny way. I ask, “Why is she tripping so much all this sudden?” The whole cycle starts again - worry, fear, research, questions, which specialist, doctor’s appointment, diagnostics, wait and watch, repeat.
All this, not to mention preparing Mya for everything that is going to happen to her. Helping her through doctor appointments, the poking, prodding, needles, wires, “pictures of her bones,” checking on her “superhero spots.” My little girl has just turned 4 years old. “Why does she have to endure more than most adults?” I ask myself. I feel overwhelmed with sadness but I have to stay strong for her.
SHE LIGHTS UP EVERYONE SHE MEETS AND HAS SO MUCH POWER IN THAT LITTLE BODY OF HERS!
And our daughter... Our beautiful, smart, kind, sassy, WARRIOR of a daughter! She gives me so much strength, courage and determination. She is so resilient (as are so many little warriors like her) and she handles things that most adults have a hard time with.
This cycle happens over and over. Sometimes we have weeks or even months where little things don’t pop up and we don’t have to question every movement, pain, groan, strange behavior and tummy ache or eye twitch. In those times, I may go hours, maybe even a whole day without thinking about my daughter’s disorder, worrying or thinking about all of the “what ifs” happening inside of her body that I can’t see.
I smile, laugh, talk with friends, cry, have bad days and good days, share posts, interact on social media, run my business, we play, our family enjoys time together, we go shopping, cook, clean, do laundry. Everything is NORMAL, as it should be. EXCEPT IT’S NOT... in between all of those normal moments something hits me. It could be a spot on her skin as we get ready, an appointment on the calendar, seeing her freeze up when another kid runs too close to her, watching her struggle a little on a step at the playground or even just a post I see from another NF parent. Sometimes it’s for no reason at all…
For clarity, I wrote about our “normal” day-to-day routine before Covid-19 happened. Now, in the time of “Safer at Home” I find myself homeschooling, doing therapy, working and trying to help Mya adjust to all this without increased anxiety and juggling this strange new way of life just like most every family in the world right now. Mya’s yearly and 6 month checkups have all been put on hold and I am left to wonder when she will get her “baseline” appointments with all her specialists again. They are stressful appointments, yes, but also reassuring to have her developmental and baseline health stats, and I am missing those appointments now. I am grateful that Mya just recently had her yearly MRI (which came back clear) and that she has seemed to have no medical issues since this pandemic started, but some parents and children are not so lucky. I’ve spoken with many other friends in the NF community whose diagnostics have been put on hold. Although this seems like no big deal to some, it’s a huge deal for a parent who was just about to find out
WE CAN ALL RELATE IN SOME WAY AND BEING THERE TO LISTEN AND SUPPORT OTHER NF PARENTS GIVES ME STRENGTH DURING A TIME WHEN THERE IS SO MUCH UNCERTAINTY.
why their baby girl is having seizures occasionally, why their little boy is having vision issues and headaches so much, a parent that has just been told their child has NF and are left with so many questions because their appts are now delayed. I also know how important safety is not just for patients but the doctors and staff at all hospitals as well. Things are hard for everyone right now and I have to remind myself of that.
Just the thought of having to bring Mya in to a hospital right now for any reason gives my anxiety. I think to myself, “Will a phone appointment be enough? If she has to go to the emergency room, what risk am I putting on her? Is she at greater risk of catching Covid-19 because of her NF?” I know many are currently going through the same thought process.
I am just grateful that our last few months have been good ones and I try to focus on that as much as possible. I also reach out the others around me in the NF community who are in my position as well. Our situations may be different but we can all relate in some way and being there to listen and support other NF parents gives me strength during a time when there is so much uncertainty.
I struggle every day with this anxiety.
I am learning to cope with my daughter’s diagnosis and making sure she gets the best possible care. I find myself hypersensitive to the struggles and ailments she endures and some days I am drowning in a pool of tears because I’ve lost my way. I dream every day that this picture I have just painted for you is no longer our reality. That when something happens to our little girl we will have answers, treatments that work and most of all A CURE. Spreading awareness and funding of NF research is so important to my baby, our family and so many others we’ve had the honor to build relationships with (most of them amazing young children like Mya). It could bring us closer to treating with medications (like Selumetinib that was just FDA approved!), more support and one day even a world without this awful disorder.
I can’t fix everything. I can’t know everything. I’m still trying to come to terms with that and one day I will feel like I can handle it all better. One day I will be a little more at peace with the way life happens. Until then I will share, be honest and vulnerable and continue fighting for our daughter, advocating and fundraising for NF research.
This article is reprinted with permission from the Children’s Tumor Foundation’s website: ctf.org









 After I had a discussion with another specialist about the symptoms I was experiencing, he agreed that it was a side effect of my medication and promptly switched me to something different. In less than 24 hours, I was feeling the best I had in months. I feel like this was an oversight in my care and if there had been a clinic in place that was familiar with my case and my condition, I wouldn’t have had to endure this incredibly frustrating experience.
After I had a discussion with another specialist about the symptoms I was experiencing, he agreed that it was a side effect of my medication and promptly switched me to something different. In less than 24 hours, I was feeling the best I had in months. I feel like this was an oversight in my care and if there had been a clinic in place that was familiar with my case and my condition, I wouldn’t have had to endure this incredibly frustrating experience.

 WHAT WAS THE EXPERIENCE OF GOING TO A MULTI-DISCIPLINARY NF CLINIC?
WHAT WAS THE EXPERIENCE OF GOING TO A MULTI-DISCIPLINARY NF CLINIC?





 Now that we have a second child, we’re constantly monitoring and analyzing our youngest for signs that something may be wrong, despite the doctors saying there’s only a 1% chance that she has NF. It really takes a conscious effort to not be anxious or overly critical all the time. We had an appointment with our youngest daughter’s pediatrician, and our doctor asked if we had any questions. I said, “What’s normal now?” She began to explain what seizures look like, but I understood that. When your child is having upwards of sixty seizures a day, it isn’t hard to identify them. I wanted to know what normal looks like now for us. And she had no answer for us at first. But she helped explain what movements indicate a trip to Children’s [Hospital] and what are just regular movements(because they can be hard to distinguish).
Now that we have a second child, we’re constantly monitoring and analyzing our youngest for signs that something may be wrong, despite the doctors saying there’s only a 1% chance that she has NF. It really takes a conscious effort to not be anxious or overly critical all the time. We had an appointment with our youngest daughter’s pediatrician, and our doctor asked if we had any questions. I said, “What’s normal now?” She began to explain what seizures look like, but I understood that. When your child is having upwards of sixty seizures a day, it isn’t hard to identify them. I wanted to know what normal looks like now for us. And she had no answer for us at first. But she helped explain what movements indicate a trip to Children’s [Hospital] and what are just regular movements(because they can be hard to distinguish). Hazelyn’s milestones now are surrounded with more happiness then McKenzie’s. When Hazelyn smiles, we’re so happy to see this milestone. But with MacKenie it was “there’s a smile but she should have smiled months ago” and it was filled with much more sadness. Now we’re just able to enjoy these moments.
Hazelyn’s milestones now are surrounded with more happiness then McKenzie’s. When Hazelyn smiles, we’re so happy to see this milestone. But with MacKenie it was “there’s a smile but she should have smiled months ago” and it was filled with much more sadness. Now we’re just able to enjoy these moments.


 A fashion blogger, influencer, and stylist, Arooj is known online for her distinct baggy clothing style and put together outfits. Though I had followed her Instagram at @vogue_wonders, where Arooj currently has over 10,000 followers, I wasn’t sure what to expect when we spoke. I shouldn’t have been nervous. From the moment we get on the call, her positive energy and sunny outlook was clear: Arooj seems to find inspiration everywhere she looks. “I find inspiration in what I read, what I see, what I look at, magazines, fashion trends already out there, and more – I try to find as much inspiration as I can on a daily basis to help people on my platform.”
A fashion blogger, influencer, and stylist, Arooj is known online for her distinct baggy clothing style and put together outfits. Though I had followed her Instagram at @vogue_wonders, where Arooj currently has over 10,000 followers, I wasn’t sure what to expect when we spoke. I shouldn’t have been nervous. From the moment we get on the call, her positive energy and sunny outlook was clear: Arooj seems to find inspiration everywhere she looks. “I find inspiration in what I read, what I see, what I look at, magazines, fashion trends already out there, and more – I try to find as much inspiration as I can on a daily basis to help people on my platform.” “My main style consists of oversized fitting clothes which I share on my Instagram. But in working in the fashion industry [in roles spanning from scouting to digital content], I want to show that no matter what you’ve got, you can be who you want to be. I’ve always been interested in fashion and intrigued by the way clothing fits on our bodies, and how it becomes a representation of who we are. It’s not just about clothing – it’s about expression.” Arooj didn’t start off using her platform this way – originally, it was simply to share her own style.
“My main style consists of oversized fitting clothes which I share on my Instagram. But in working in the fashion industry [in roles spanning from scouting to digital content], I want to show that no matter what you’ve got, you can be who you want to be. I’ve always been interested in fashion and intrigued by the way clothing fits on our bodies, and how it becomes a representation of who we are. It’s not just about clothing – it’s about expression.” Arooj didn’t start off using her platform this way – originally, it was simply to share her own style. Arooj eventually became shortlisted for a Cosmopolitan Award for her sharp style sense. And yet, while this was exciting, she couldn’t help but regret that no one following her platform knew the true story behind her baggy attire. “It was then I started to feel like I couldn’t accept it; I felt like a bit of a fraud – because no one knew my real story. I felt like I was hiding. I wanted to achieve something but I wanted to be authentic as I achieved it.”
Arooj eventually became shortlisted for a Cosmopolitan Award for her sharp style sense. And yet, while this was exciting, she couldn’t help but regret that no one following her platform knew the true story behind her baggy attire. “It was then I started to feel like I couldn’t accept it; I felt like a bit of a fraud – because no one knew my real story. I felt like I was hiding. I wanted to achieve something but I wanted to be authentic as I achieved it.” NF is often a hidden condition – so many afflicted by it hide the fact that they have it, which can lead to a lack of general awareness about it. Even though NF1 is found in roughly one out of every 3,000 individuals, there are few public figures who have admitted to having the genetic disorder. Arooj has given many people with NF a woman to look up; a figure in the public eye who is going through the same challenges they are. “I’ve had people write me saying ‘Wow, I’ve never seen a person with NF in the mainstream media.’ It’s kind of crazy to me, because so many people deal with it. For me, I’m just happy I can use my voice to spread the word. When British Vogue mentioned me in an article, it meant a lot to me – to see huge publications pick up my story and share it with their readership has been amazing. More people are learning about what NF means and how common it is.”
NF is often a hidden condition – so many afflicted by it hide the fact that they have it, which can lead to a lack of general awareness about it. Even though NF1 is found in roughly one out of every 3,000 individuals, there are few public figures who have admitted to having the genetic disorder. Arooj has given many people with NF a woman to look up; a figure in the public eye who is going through the same challenges they are. “I’ve had people write me saying ‘Wow, I’ve never seen a person with NF in the mainstream media.’ It’s kind of crazy to me, because so many people deal with it. For me, I’m just happy I can use my voice to spread the word. When British Vogue mentioned me in an article, it meant a lot to me – to see huge publications pick up my story and share it with their readership has been amazing. More people are learning about what NF means and how common it is.” Still, Arooj is incredibly humble when I congratulate her for her bravery and for setting an example for others. “I’m not perfect”, she admits. “What works for me might not work for everybody else. I think the first step is trying to accept your condition, and knowing that it’s not the end. The first stage for me has always been acceptance; understanding myself and my needs. For those newly diagnosed, I would just remind people to not let NF put up barriers for who you want to be in the world. We are so much more than our conditions as people. We have so much more to achieve.”
Still, Arooj is incredibly humble when I congratulate her for her bravery and for setting an example for others. “I’m not perfect”, she admits. “What works for me might not work for everybody else. I think the first step is trying to accept your condition, and knowing that it’s not the end. The first stage for me has always been acceptance; understanding myself and my needs. For those newly diagnosed, I would just remind people to not let NF put up barriers for who you want to be in the world. We are so much more than our conditions as people. We have so much more to achieve.” It also doesn’t have to be too planned, or part of a routine. Rather, Arooj speaks to the importance of generally trying to take it day-by-day. “I don’t necessarily have a routine. I think each day we learn, we see what’s good for us, what’s not good for us. I try to get an early night, but it doesn’t always happen. You can’t always know what the future holds, so I take it day by day. My advice to others is: take each day as it comes, but don’t have expectations. Be grateful for your experiences and opportunities and stay positive. When you’re positive you can be the best person of yourself, and not let anything stop you”.
It also doesn’t have to be too planned, or part of a routine. Rather, Arooj speaks to the importance of generally trying to take it day-by-day. “I don’t necessarily have a routine. I think each day we learn, we see what’s good for us, what’s not good for us. I try to get an early night, but it doesn’t always happen. You can’t always know what the future holds, so I take it day by day. My advice to others is: take each day as it comes, but don’t have expectations. Be grateful for your experiences and opportunities and stay positive. When you’re positive you can be the best person of yourself, and not let anything stop you”. “It’s always mindset over matter” Arooj explains. “It’s easier said than done, but if you can start developing a stronger mindset, the world is your oyster. The minute I get up and be positive and do things, my life will change. I’ve tried to take on an attitude of recognizing how lucky I am – how lucky I am for healthcare, and for the life I do have. I’m lucky to have great friends, great family – and lucky to have a voice.” Of course, there are challenges. There are good days and bad. But building a community online, an extended network of supporters and friends, has helped Arooj stay strong and keep moving forward.
“It’s always mindset over matter” Arooj explains. “It’s easier said than done, but if you can start developing a stronger mindset, the world is your oyster. The minute I get up and be positive and do things, my life will change. I’ve tried to take on an attitude of recognizing how lucky I am – how lucky I am for healthcare, and for the life I do have. I’m lucky to have great friends, great family – and lucky to have a voice.” Of course, there are challenges. There are good days and bad. But building a community online, an extended network of supporters and friends, has helped Arooj stay strong and keep moving forward. “One thing I want to be clear about” Arooj states “is that I haven’t beat NF – I’ve just accepted it". I’m not some superwoman who has suddenly overcome it. What I have tried to do is be open with it. Accepting and overcoming are two different things: but what has helped me is hearing stories of other people and knowing that I’m not alone.”
“One thing I want to be clear about” Arooj states “is that I haven’t beat NF – I’ve just accepted it". I’m not some superwoman who has suddenly overcome it. What I have tried to do is be open with it. Accepting and overcoming are two different things: but what has helped me is hearing stories of other people and knowing that I’m not alone.” Brittany McGillivray is an editor and content strategist based in Vancouver BC. She has an MA in New Media and Digital Culture from the University of Amsterdam and a BA in Literature from McGill. As an avid reader, writer, and aspiring poet, she cares most about community, feminism, and giving a platform to all voices.
Brittany McGillivray is an editor and content strategist based in Vancouver BC. She has an MA in New Media and Digital Culture from the University of Amsterdam and a BA in Literature from McGill. As an avid reader, writer, and aspiring poet, she cares most about community, feminism, and giving a platform to all voices.
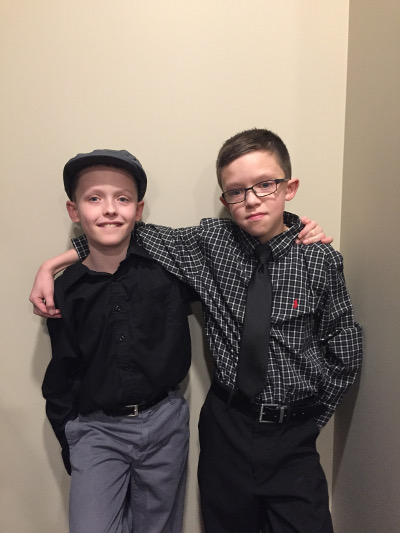


 This is my son Crew and he has a genetic disorder called Neurofibromatosis 1 (NF1). NF has greatly impacted his life. At age 2.5 years old Crew has had at least 5 MRIs under sedation, he has 8 different doctors or specialists, too many appointments to count, he has tumors in his mouth, cheek, near his brain stem and neck. The tumors have caused his tongue to be asymmetrical to the extent of the center of his tongue being on the left side. His speech is being greatly affected and has started Speech Therapy. He often accidentally bites his tongue and gets frustrated when others can not understand him. The tumors have caused his parotid gland in his cheek to be blocked and will be needing Botox injections under sedation. Due to the tumor on the trigeminal nerve, every time when he chews food red flushing occurs on his right cheek that sometimes goes into his ear, eyelid and hairline. Sometimes when his skin flushes his right eye will water. Crew has been taking a chemotherapy medication since 11/29/16. Sometimes the meds make his stomach feel upset or gives him headaches.
This is my son Crew and he has a genetic disorder called Neurofibromatosis 1 (NF1). NF has greatly impacted his life. At age 2.5 years old Crew has had at least 5 MRIs under sedation, he has 8 different doctors or specialists, too many appointments to count, he has tumors in his mouth, cheek, near his brain stem and neck. The tumors have caused his tongue to be asymmetrical to the extent of the center of his tongue being on the left side. His speech is being greatly affected and has started Speech Therapy. He often accidentally bites his tongue and gets frustrated when others can not understand him. The tumors have caused his parotid gland in his cheek to be blocked and will be needing Botox injections under sedation. Due to the tumor on the trigeminal nerve, every time when he chews food red flushing occurs on his right cheek that sometimes goes into his ear, eyelid and hairline. Sometimes when his skin flushes his right eye will water. Crew has been taking a chemotherapy medication since 11/29/16. Sometimes the meds make his stomach feel upset or gives him headaches.